I haven't posted for a long time.
I survived intern year. I survived residency, and through that crucible forged bonds that I'm going to have for the rest of my life.
I did a fellowship in urological oncology/robotic surgery as well - clinically one of the toughest years of my life but immensely satisfying.
I have a job in private practice, with a robust practice, great partners, doing cases I love, and a fantastic quality of life letting me spend time with what matters most - my two beautiful girls (currently ages 4.5 and 2.5). My wife is pregnant with a third on the way!
It was perfect.
I'm writing this post from a hospital room, much as my previous posts were written. But this is different.
I'm not a doctor right now. I'm not a patient. I'm a terrified father.
My youngest baby has been diagnosed with leukemia. Acute lymphoblastic leukemia.
The dark room I'm typing from is illuminated by the green glow of the IV pump that is currently transfusing her blood. Two days ago I watched my baby roll back into the operating room, the same walk I have made thousands of times, but always as the surgeon. I lost complete control over her while a team of doctors put in a port and gave her spinal chemotherapy.
The last week has been the worst week of my life. Nothing can prepare you for the pain of having a child diagnosed with cancer. I wish I had the ability to write down what I was feeling, but I can't.
There is so much anger. Anger that all those years sacrificed in residency and fellowship to provide the best for my family - and in my first year of practice this happens.
So much fear. Childhood leukemia has a cure rate of >90%. But there is a ten percent chance my little angel doesn't make it. I can barely type out that sentence.
So much sadness. My daughter is two and a half - she needs two years of chemotherapy. I've been living this for 7 days and can't fathom how we are going to make it two more years. And my poor older daughter is already feeling neglected, but what can we do? And my unborn baby, due this upcoming March, will always be second fiddle.
Back to anger. I missed most of the childhood of my first two kids due to residency/fellowship. I wanted to be there for this third baby, experience all the small moments. I've lost that.
Now guilt. The above sentence is just selfish. My baby in the hospital needs me, and she's scared and suffering. She's so scared. How can I even think of myself?
And the worst is knowledge that things will never be normal again. For the next ten years (it takes that long to be fully declared cured) every blood test, every fall, every cold will invoke a sense of dread. The spectre of cancer returning will hang over me every day. And - if she is cured - chemo has its side effects. Decreased neurocognition, peripheral neuropathy, risks secondary malignancy, cardiac effects etc. How much does she understand? Does a toddler who spends week in the hospital, who is hobbled by chemo, who has her growth interrupted by steroids grow up to be well rounded? I don't care if she's not a physicist or lawyer or whatever - I just want her to be happy. I would do anything, give anything, trade anything, sacrifice anything for her to get through this unscathed.
life as a surgical resident
Surgery, urology, intern year, residency, leukemia, pediatric acute lymphoblastic leukemia, ALL
Wednesday, November 6, 2019
Saturday, May 10, 2014
donuts
When I was an intern last year, I spent a month rotating on the transplant service. We do about 3-4 kidney transplants a week, so taking care of them became relatively routine. A good portion of our patients who needed transplants had renal failure from diabetes, which is basically uncontrolled blood sugars.
So I had the pleasure of taking care of one such patient near the end of my transplant rotation. She had been given the gift of a kidney, and with proper care she might be able to avoid going back on dialysis for 10, 12 years. A precious gift, which she clearly didn't care about...
I get a page the morning of her second day in the hospital. which was less that 48 hours previously she had gotten the kidney. The kidney was working great, which was why I was so surprised about the page. Our nurses document everything in the computer, and her documentation reads as follows:
"Patient caught eating donuts in room. She apologized when blood glucose was found to be 403 [very hight!]. 12 units of Lispro given, patient thoroughly lectured, Dr. *** informed. Will continue to monitor. Donuts confiscated."
Mind blowing. We couldn't have found a better home for this kidney?
So I had the pleasure of taking care of one such patient near the end of my transplant rotation. She had been given the gift of a kidney, and with proper care she might be able to avoid going back on dialysis for 10, 12 years. A precious gift, which she clearly didn't care about...
I get a page the morning of her second day in the hospital. which was less that 48 hours previously she had gotten the kidney. The kidney was working great, which was why I was so surprised about the page. Our nurses document everything in the computer, and her documentation reads as follows:
"Patient caught eating donuts in room. She apologized when blood glucose was found to be 403 [very hight!]. 12 units of Lispro given, patient thoroughly lectured, Dr. *** informed. Will continue to monitor. Donuts confiscated."
Mind blowing. We couldn't have found a better home for this kidney?
Tuesday, March 11, 2014
The Med Student Chronicles: Daylight savings time is not my friend
As a urologist, kidney's are part of my field. In fact, as I write this post I am sitting in the library waiting for a transplant to get started (the transplant surgeons do the artery and vein, and this particular patient has complex urological anatomy so we do the ureter).
It takes me back to my surgery rotation of 3rd year of med school. I knew pretty early that surgery was something I wanted to go in to and I was pretty excited. I started off the rotation on the surgical oncology service, and it was pretty busy. Each morning you came in around 4:30AM, and we ended up being there till about 7/8 most nights. Exhausting.
By the time Friday rolled around you were ready for the weekend. Unfortunately our school wanted us to get a feel for what a surgery residency was like, so they mandated weekend call. I had the luck of being the first one to take a weekend call, so that weekend I started Saturday at 5:30am,and was on till about Sunday at noon or so. I was honestly dreading it, but it is what it is and was hopeful I'd see some interesting trauma's or cases.
The day went by pretty smoothly, a few small trauma's but nothing to exciting. Around 8pm we headed down to the residents lounge and started watching some basketball. Around 9, the transplant resident who was on call rolls in and lets the team know they have a kidney coming in, and then looks at me and asks if I want to scrub in. Normally the residents let the medical students go sleep a bit around 10/11 unless any traumas came in, but this was a once in a lifetime chance! I was SO excited, and said of course I would like to scrub and help. I'd seen some pretty cool cases on the surgical oncology service, but a kidney transplant trumps all that. To take an organ and transplant it into someone else...crazy.
Anyways it takes about two hours for the kidney and the patient to make it into the OR, and by the time we finally make incision its about 11:30 on saturday night, already 18 hours into my shift with another 12 to go. Didn't matter, I was pumped, ready to go. Gonna watch a kidney transplant!
Everything starts off great. Nice big incision. As a brief aside, the reason as a medical student you always think about the incision is because really that's the only thing you get to do. In the days of laparoscopy with only a few small incisions, there aren't many opportunities for med students to practice closing. Thus we always look forward to big incisions. But anyways back to the case.
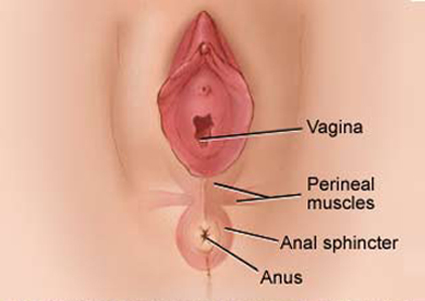
The attending and resident dissect down through the subcutaneous tissue, down to the bladder. This is what it looked like at that point:
I had a pretty good view of what was going on, and had a hand on a retractor. Life is good.
It takes me back to my surgery rotation of 3rd year of med school. I knew pretty early that surgery was something I wanted to go in to and I was pretty excited. I started off the rotation on the surgical oncology service, and it was pretty busy. Each morning you came in around 4:30AM, and we ended up being there till about 7/8 most nights. Exhausting.
By the time Friday rolled around you were ready for the weekend. Unfortunately our school wanted us to get a feel for what a surgery residency was like, so they mandated weekend call. I had the luck of being the first one to take a weekend call, so that weekend I started Saturday at 5:30am,and was on till about Sunday at noon or so. I was honestly dreading it, but it is what it is and was hopeful I'd see some interesting trauma's or cases.
The day went by pretty smoothly, a few small trauma's but nothing to exciting. Around 8pm we headed down to the residents lounge and started watching some basketball. Around 9, the transplant resident who was on call rolls in and lets the team know they have a kidney coming in, and then looks at me and asks if I want to scrub in. Normally the residents let the medical students go sleep a bit around 10/11 unless any traumas came in, but this was a once in a lifetime chance! I was SO excited, and said of course I would like to scrub and help. I'd seen some pretty cool cases on the surgical oncology service, but a kidney transplant trumps all that. To take an organ and transplant it into someone else...crazy.
Anyways it takes about two hours for the kidney and the patient to make it into the OR, and by the time we finally make incision its about 11:30 on saturday night, already 18 hours into my shift with another 12 to go. Didn't matter, I was pumped, ready to go. Gonna watch a kidney transplant!
Everything starts off great. Nice big incision. As a brief aside, the reason as a medical student you always think about the incision is because really that's the only thing you get to do. In the days of laparoscopy with only a few small incisions, there aren't many opportunities for med students to practice closing. Thus we always look forward to big incisions. But anyways back to the case.
The attending and resident dissect down through the subcutaneous tissue, down to the bladder. This is what it looked like at that point:
I had a pretty good view of what was going on, and had a hand on a retractor. Life is good.
Suddenly it all changed. See a kidney transplant essentially boils down to three major steps. Hook up the artery, hook up the vein, and hook up the ureter. The tricky part about kidney transplants is that sometimes you are working deep in the pelvis, and its tough to see and get an angle that deep in a patient's body. To compensate, the surgeon's turn their body and angle themselves to look down.
This is what it looked like
Literally all I could see was the residents back. He had a hairy back, with tufts of hair poking out above his scrub top.
I repositioned, and if I stood on the tip of my toes and totally angled my body and leaned over the table I could catch a glimpse of what was happening!
Ohhhh but it hurt my back so much. That lasted about five minutes, and I repositioned and once again could only see my residents back.
I start to nod off. The thing with being scrubbed is you have to keep your hands above your waist at all times, and there it nothing to lean on. It's really awkward, and by this time its 1:30 in the morning and I've been up for 20 hours. I needed to distract myself to stay awake.
I started counting my resident's back hairs. It seemed like an impossible task, but I was determined to get a number. That worked for about 15 minutes, but then the counting made me sleepy.
Its 1:45 in the morning. When will this night end???
I start to think I could have been in bed right now. There is literally nowhere else in the world I'd rather be. If this was torture I would have broken a long time ago.
Look back at the clock. Its 1:55. Time seems to have stopped. This needs to end. I hear someone mention bleeding, but at this point I'm in a delirious in between state with no concept of words.
I can't stop staring at the clock.
1:59
I watch the seconds hand turn the corner, past the thirty. I can't believe its almost two in the morning, and I could have been in a nice bed. I wish I could see something, anything. The second hand turns, turns, and bam it's 2:00
The clock stops. The minutes hand starts rolling backwards.
What is happening? I rack my brain looking for an answer. I'm sure in my sleep addled mindset I'm hallucinating. Throughout all this, the minutes hand keeps rolling backwards, and then all of a sudden stops.
The clock shows 1:00.
It just doesn't make sense. It was just 2! How could it be 1? And then it hits me.
Its daylight savings time. That beautiful time of year, where the whole nation rejoices in a free hour of sleep. Well let me tell you my friends, nothing is free. That night daylight savings time equaled an extra hour of call, an extra hour of torture.
And to top it off, at the end of the case when it was time to close? The attending says "Its been a long night, why don't you just use staples instead of suturing and be done with it"
Tuesday, February 25, 2014
The Med Student Chronicles: My first vaginal exam
It was my first rotation of third year. The first two years of med school are your preclinical years, you spend hours in the classroom and at home studying and getting the building blocks you use for the clinical years.
Second year culminates with the USMLE step I exam, which is kind of a final exam for the first two years of preclinical training. After passing it, you are graduated to third year and get to be on the floor with real patients. As all of us went to med school to be physicians, to interact with people is something you definitely look forward to. Our school had a lottery system for third year rotations, and I had one of the last numbers and little control over my schedule. I got stuck with OB-GYN as my first rotation which I was actually ok with it because I knew it was something I probably wouldn't be interested in.
OB-GYN is an interesting rotation. It's something that as a medical student and future physician its good to know the basics of, however most women aren't fans of letting a med student examining them (shocking!). It's this awkward interplay between wanting to do and see stuff, and then getting constantly rejected. Especially being the first rotation of third year, we were totally green and it showed.
My first week was on ultrasound and urogyn, which was pretty straightforward. Then I went to the hellhole that is labor and delivery. There were two med students at a time on L&D, one who would work 6am to 6pm and the other one would be on 6pm to 6am. L&D is just always busy, there would be 10-12 women at a time in some form or another of labor. The service was run by a chief resident and two junior residents on at all times, along with the attending and the med students. My chief resident while I was on nights was this really awesome guy, we got along great. Two guys standing strong in a sea of estrogen, or something like that.
Anyways, we did a ton of vaginal exams on L&D. Every couple of hours the residents would examine the patients and see how dilated their cervix was, and how close the baby was to popping out. My chief was pretty good about getting me involved, and as it was still early in the rotation I hadn't been horribly scarred yet and I wanted to do stuff. Some patients were not good candidates, but their was one lady who just didn't care. She was this huge (>300 pounds) Hispanic lady. She had a few kids before, and you could tell she just wanted to pop this one out and get home. Her first exam of the night showed her to be a few centimeters dilated, and she was probably going to deliver later that evening.
So the chief and I are hanging out in the call room, killing time waiting for someone to be ready to deliver. Around 2am we decide to tour the floor and see how everyone is progressing. He wanted to examine her, and after doing a couple with me earlier on rounds he trusted me enough to do the exam and let me tell him how far along she was. I have to mention, and this becomes relevant, is that he had chewed me out on the previous exam for staring too much. You see, in order to see how dilated their cervix is, we obviously have to do a vaginal exam. And having done very few of them, I would have the patients spread their legs, stare intently at their vagina while I tried to find the opening and get in there. Ironically enough, after spending years trying to get closer to vaginas, when finally given the opportunity I had a hard time finding em. Nonetheless, my chief hammered home the point that, while doing these exams, we aren't looking for anything but are just "feeling" how dilated their cervix is.
So back to our friend. We get to her room, and he sends me in first to examine her while he hangs out in the back. She speaks no English, and the extent of my Spanish is to tell her "yo no hablo espanol". Fortunately through a series of hand gestures I'm able to convey the message that its time for me to examine her. She spreads her legs, and I dive in. She has this vacant "been there, done that" look to her. This time I'm mindful not to stare, and choose to stare at the double chin on her double chin. Her legs are so big that my hand is engulfed, I feel like I'm a engulfed in a giant cavern of darkness.
I'm feeling around, feeling around trying to find her vaginal opening. It should take about 5 seconds to find the opening and get in, I'm approaching 20 seconds which is basically an eternity to be rooting around in someone's groin. My chief is getting antsy, and I hear him clear his throat.
This is my white whale. This is my Everest. I will find this vagina I tell myself. I redouble my efforts, and slide my hand down, down, down trying to find it. As I'm losing hope, as I feel my opportunity slipping away all of a sudden I feel an opening.
I'm in!
I confidently stick my finger in the hole I've found, ready to measure her cervix. As my finger slides in she shrieks and jumps up on the bed. At first, I'm confused, but then the reality quickly dawns on me. I'm in the wrong hole
You see, the anus lies right below the vagina in females. I had managed to entirely miss the vagina, and ended up doing a rectal sans lube.
As soon as I realized this, I withdrew my fingers. We locked gazes, and just stared at each other in utter shock. I silently begged her not to say anything, realizing that even if she wanted to neither of us spoke Spanish. I also was in a little bit of a dilemma regarding her vaginal exam. I didn't want to stick my poop covered fingers into her vagina, infecting her baby. I also didn't want to tell my resident what happened as I knew for the rest of my ob gyn rotation I would never live this down. I came up with a third option, and told him that I was having trouble doing the exam and if he could check himself. He gladly gloved up, and in about 5 seconds did a thorough and competent exam.
As I backpedaled out of the room, we briefly made eye contact again and she gave a little head shake. I'll never know for sure what she was thinking at that moment, but I like to think she was saying "thank you for trying, and your secret is safe with me".
Or she may have been saying "get the *%& out of my room, and never come back".
I'll never know.
Thursday, January 2, 2014
Mistakes
This is going to be a long post...I apologize
Everyone makes mistakes. Hell the internet is littered with quotes from famous people about mistakes.
"A person who never made a mistake never tried anything new."
- Some guy named Einstein
"A mistake is always forgivable, rarely excusable and always unacceptable."
- Robert Fripp
And it goes on.
Mistakes are different in the medical community. I alluded to it an earlier post. An athlete makes a mistake, his team might lose. An accountant makes a number, he has to make an embarrassing phone call to a client to fix his wrong.
A surgeon makes a mistake, and it can cost someone their life.
I'm by no means the first, nor will I be even close to the last to being a doctor - honestly barely a doctor a fresh graduate out of medical school - to make a mistake that has led to irreversible harm. In the surgical community, we even acknowledge that such mistakes exist and discuss them in a setting that is theoretically safe from judgement - the weekly M&M (morbidity and mortality) conference. The idea is that mistakes, as in any profession, happen and our goal should be to learn from them. This concept in itself is troubling, in essence it leads to a dichotomy between what physicians should strive to be, perfect, and the reality that like any other profession we will make mistakes.
This has been discussed previously. When I was a fourth year medical student a friend of mine introduced me to Atul Gawande, a surgeon who has written numerous books of his experiences in training. He actually has dedicated books to the topic, with a book called Complications, and another called The Checklist Manifesto that delve into the topics of mistakes and how to prevent them. Definitely great reading if you have time.
But reading about mistakes is one thing. I had read his books before starting my intern year. I knew residents who had made mistakes as medical students. It wasn't a big deal at the time. I think thats human nature. Despite our best intentions to empathize with other people, to put ourselves in their shoes and understand what they are going to we just can't. Very few people have that ability. Instead we recognize they are going through something, try and understand and be supportive, and forget about it 5 minutes later.
So enough rambling. I started intern year off on night float, made some very small mistakes that really were inconsequential, and overall had a great start to the year. I next went to colorectal, a notoriously busy service. I knew it was going to be long hours (and it was), but I loved it. I was always tired and overworked, but if you worked hard and could get to the OR in the afternoon the fellow was great about letting interns do alot. Great experience.
We rounded early on colorectal, 6am. This means I would be coming in around 4:30 to get numbers, and see 6-12 patients before rounds. Sometimes notes would need to be done too before rounds. Grueling, but I got used to it.
Every Wednesday we have conference from 7-8 AM. We did our AM rounds in the morning as normal. Nothing exciting, and we headed to conference. Right after conference I sit down with the fellow and the senior resident to run the list when I get a page that one of our patients, lets call her AT, is short of breath. Ok no big deal, I head over to the floor to see whats going on. She's a very pleasant 70 something year old lady who had part of her colon removed for recurrent diverticulitis. The case was straightforward, and she was post-op day #2. We had probably planned to send her home the following day. When I saw her I was shocked at how short of breath she actually was. That morning at 5am when I had seen her she was so comfortably. One of the immediate post operative causes of shortness of breath that you always worry about is a clot in the leg that formed from not walking enough after surgery and that clot breaking off and traveling to the lungs, something called a pulmonary embolus. The quick and easy way to get an idea of whats going on non-invasively is do something called a duplex scan, which I order. Her vital signs were completely stable so I wasn't really concerned about something catastrophic.
I leave her room, call my senior resident to run the plan by him, and start walking to our resident room. As I'm walking there I think in my head
"She's on heparin, right"?
Heparin is a blood thinner that we commonly use after surgery because it can help prevent blood clots in the legs. It does come with a risk of bleeding, but generally you can fix that whereas the clots/emboli can be significantly more devastating. During rounds the morning before (Tue), my attending had asked me if she was on heparin. I honestly had no idea, but told him I'd check and if she wasn't I'd start it.
"Did I remember to do that"?
I start to panic a little, and kind of half run to the resident room. I have to check the computer and see if its ordered. I log in, look at her orders.
Its not there.
I forgot...
My heart sinks. I start hyperventilating. And honestly - I'm pretty laid back most of the time. I didn't know what was happening. I all the vascular lab and beg them to do the duplex right away. I plant myself in the nurses station in front of AT's room and wait for them.
As I wait, I tell myself I'm overreacting. Its not a big deal. She's probably just a little fluid overloaded. Its not going to a clot in her legs. The vascular tech arrives, goes in the room. I start to calm down. Its all going to be ok.
I pace around the nursing station, waiting for him to finish. I'm convinced its going to be nothing.
The tech walks out of the room, and I chase him down.
"Did you find anything" I ask.
"Yup, acute clot in the left femoral vein" he says, and hands me a schematic of where her clot is.
That crushing overwhelming feeling comes back. I don't know what to think. I call my senior resident, update him. He tells me to text the attending, Dr. P. I get ahold of him, and let him know that she's short of breath, and has a DVT (the leg clot) - making it likely (but not 100%) that she has a pulmonary embolus (PE). He agrees that she probably has a PE, and wants to get a special kind of CT scan to diagnose it. He also wants to start her on a heparin drip to presumptively treat her, all reasonable things to do. I tell him I'll take care of it and we hang up.
He then texts me
"Hey bladder whisperer, she was on heparin right?"
My heart sinks. "No actually she wasn't..."
"Wait, I thought I asked you to check yesterday?"
I didn't know what to say. All I said was "Honestly I forgot".
I was ready for the worst. I thought it was over. His response?
"Oh BW, that was a mistake".
Then silence
I felt terrible. He wasn't mad, he was disappointed. It all hit me like a ton of bricks. This was his patient, his license, his name on the line. This complication, regardless of who caused it, is his responsibility. And it was my fault. Already I felt like nothing because I felt responsible for AT's current shortness of breath, and now I was putting my team through this.
The rest of the day was a whirlwind. I still had 10 other post operative patients to take care of, discharges, consults etc. The thing about being busy is you don't have time to think. I just worked, and got through it.
But the day had to end at some point. I walk to work, and left around 7pm. The walk home I finally had some time to think, and thats when I started to get inside my head. I made it home and just broke down. I got no sleep that night, just tossing and turning. Around 2am I finally gave up, and headed into the hospital. The rest of the team had already moved on, new patients and new things to take care of. But for me it was all about AT. I couldn't stop thinking about her, stop checking in on her. I tried rationalizing it to myself, that despite the heparin she would have gotten it anyways. I tried shifting the blame to the other people who hadn't ordered it or caught the mistake. It stayed with me every second, every decision.
But life goes on. She did great on the heparin drip, and her shortness of breath resolved. She was bridged to coumadin, and planned to be discharged home. At the time of her discharge I stopped by her room to wish her luck and make sure everything was taken care of and we said our good byes.
At that point her husband stops me and says "I just want to thank you for everything you've done for me and my family". He gives me a firm handshake and says "If you are ever up in our neck of the woods look me up, I owe you a beer".
I looked down, because I knew if I looked him or his wife in the eyes they would see right through me. The thing is in my guilt I had made sure I came to see them multiple times a day, and basically was there for them the second they needed anything. From their standpoint, AT had developed a complication and I was on the frontline, the doctor who was with them and helped them through it. Dr. P didn't throw me under the bus and tell them it was my fault, all he had told them was it should have been ordered but mistakenly hadn't.
It broke my heart. Their was nothing i could say, and I mumbled a response back and got out of the room.
It took weeks for the numbness to resolve, and the incident has change me as a person. I've made many mistakes in my life, and will make many more. But the knowledge that I caused harm to someone, that someone may have lost their life and will certainly have some morbidity from a mistake I made lies heavy in my heart, even more than one year later.
Everyone makes mistakes. Hell the internet is littered with quotes from famous people about mistakes.
"A person who never made a mistake never tried anything new."
- Some guy named Einstein
"A mistake is always forgivable, rarely excusable and always unacceptable."
- Robert Fripp
And it goes on.
Mistakes are different in the medical community. I alluded to it an earlier post. An athlete makes a mistake, his team might lose. An accountant makes a number, he has to make an embarrassing phone call to a client to fix his wrong.
A surgeon makes a mistake, and it can cost someone their life.
I'm by no means the first, nor will I be even close to the last to being a doctor - honestly barely a doctor a fresh graduate out of medical school - to make a mistake that has led to irreversible harm. In the surgical community, we even acknowledge that such mistakes exist and discuss them in a setting that is theoretically safe from judgement - the weekly M&M (morbidity and mortality) conference. The idea is that mistakes, as in any profession, happen and our goal should be to learn from them. This concept in itself is troubling, in essence it leads to a dichotomy between what physicians should strive to be, perfect, and the reality that like any other profession we will make mistakes.
This has been discussed previously. When I was a fourth year medical student a friend of mine introduced me to Atul Gawande, a surgeon who has written numerous books of his experiences in training. He actually has dedicated books to the topic, with a book called Complications, and another called The Checklist Manifesto that delve into the topics of mistakes and how to prevent them. Definitely great reading if you have time.
But reading about mistakes is one thing. I had read his books before starting my intern year. I knew residents who had made mistakes as medical students. It wasn't a big deal at the time. I think thats human nature. Despite our best intentions to empathize with other people, to put ourselves in their shoes and understand what they are going to we just can't. Very few people have that ability. Instead we recognize they are going through something, try and understand and be supportive, and forget about it 5 minutes later.
So enough rambling. I started intern year off on night float, made some very small mistakes that really were inconsequential, and overall had a great start to the year. I next went to colorectal, a notoriously busy service. I knew it was going to be long hours (and it was), but I loved it. I was always tired and overworked, but if you worked hard and could get to the OR in the afternoon the fellow was great about letting interns do alot. Great experience.
We rounded early on colorectal, 6am. This means I would be coming in around 4:30 to get numbers, and see 6-12 patients before rounds. Sometimes notes would need to be done too before rounds. Grueling, but I got used to it.
Every Wednesday we have conference from 7-8 AM. We did our AM rounds in the morning as normal. Nothing exciting, and we headed to conference. Right after conference I sit down with the fellow and the senior resident to run the list when I get a page that one of our patients, lets call her AT, is short of breath. Ok no big deal, I head over to the floor to see whats going on. She's a very pleasant 70 something year old lady who had part of her colon removed for recurrent diverticulitis. The case was straightforward, and she was post-op day #2. We had probably planned to send her home the following day. When I saw her I was shocked at how short of breath she actually was. That morning at 5am when I had seen her she was so comfortably. One of the immediate post operative causes of shortness of breath that you always worry about is a clot in the leg that formed from not walking enough after surgery and that clot breaking off and traveling to the lungs, something called a pulmonary embolus. The quick and easy way to get an idea of whats going on non-invasively is do something called a duplex scan, which I order. Her vital signs were completely stable so I wasn't really concerned about something catastrophic.
I leave her room, call my senior resident to run the plan by him, and start walking to our resident room. As I'm walking there I think in my head
"She's on heparin, right"?
Heparin is a blood thinner that we commonly use after surgery because it can help prevent blood clots in the legs. It does come with a risk of bleeding, but generally you can fix that whereas the clots/emboli can be significantly more devastating. During rounds the morning before (Tue), my attending had asked me if she was on heparin. I honestly had no idea, but told him I'd check and if she wasn't I'd start it.
"Did I remember to do that"?
I start to panic a little, and kind of half run to the resident room. I have to check the computer and see if its ordered. I log in, look at her orders.
Its not there.
I forgot...
My heart sinks. I start hyperventilating. And honestly - I'm pretty laid back most of the time. I didn't know what was happening. I all the vascular lab and beg them to do the duplex right away. I plant myself in the nurses station in front of AT's room and wait for them.
As I wait, I tell myself I'm overreacting. Its not a big deal. She's probably just a little fluid overloaded. Its not going to a clot in her legs. The vascular tech arrives, goes in the room. I start to calm down. Its all going to be ok.
I pace around the nursing station, waiting for him to finish. I'm convinced its going to be nothing.
The tech walks out of the room, and I chase him down.
"Did you find anything" I ask.
"Yup, acute clot in the left femoral vein" he says, and hands me a schematic of where her clot is.
That crushing overwhelming feeling comes back. I don't know what to think. I call my senior resident, update him. He tells me to text the attending, Dr. P. I get ahold of him, and let him know that she's short of breath, and has a DVT (the leg clot) - making it likely (but not 100%) that she has a pulmonary embolus (PE). He agrees that she probably has a PE, and wants to get a special kind of CT scan to diagnose it. He also wants to start her on a heparin drip to presumptively treat her, all reasonable things to do. I tell him I'll take care of it and we hang up.
He then texts me
"Hey bladder whisperer, she was on heparin right?"
My heart sinks. "No actually she wasn't..."
"Wait, I thought I asked you to check yesterday?"
I didn't know what to say. All I said was "Honestly I forgot".
I was ready for the worst. I thought it was over. His response?
"Oh BW, that was a mistake".
Then silence
I felt terrible. He wasn't mad, he was disappointed. It all hit me like a ton of bricks. This was his patient, his license, his name on the line. This complication, regardless of who caused it, is his responsibility. And it was my fault. Already I felt like nothing because I felt responsible for AT's current shortness of breath, and now I was putting my team through this.
The rest of the day was a whirlwind. I still had 10 other post operative patients to take care of, discharges, consults etc. The thing about being busy is you don't have time to think. I just worked, and got through it.
But the day had to end at some point. I walk to work, and left around 7pm. The walk home I finally had some time to think, and thats when I started to get inside my head. I made it home and just broke down. I got no sleep that night, just tossing and turning. Around 2am I finally gave up, and headed into the hospital. The rest of the team had already moved on, new patients and new things to take care of. But for me it was all about AT. I couldn't stop thinking about her, stop checking in on her. I tried rationalizing it to myself, that despite the heparin she would have gotten it anyways. I tried shifting the blame to the other people who hadn't ordered it or caught the mistake. It stayed with me every second, every decision.
But life goes on. She did great on the heparin drip, and her shortness of breath resolved. She was bridged to coumadin, and planned to be discharged home. At the time of her discharge I stopped by her room to wish her luck and make sure everything was taken care of and we said our good byes.
At that point her husband stops me and says "I just want to thank you for everything you've done for me and my family". He gives me a firm handshake and says "If you are ever up in our neck of the woods look me up, I owe you a beer".
I looked down, because I knew if I looked him or his wife in the eyes they would see right through me. The thing is in my guilt I had made sure I came to see them multiple times a day, and basically was there for them the second they needed anything. From their standpoint, AT had developed a complication and I was on the frontline, the doctor who was with them and helped them through it. Dr. P didn't throw me under the bus and tell them it was my fault, all he had told them was it should have been ordered but mistakenly hadn't.
It broke my heart. Their was nothing i could say, and I mumbled a response back and got out of the room.
It took weeks for the numbness to resolve, and the incident has change me as a person. I've made many mistakes in my life, and will make many more. But the knowledge that I caused harm to someone, that someone may have lost their life and will certainly have some morbidity from a mistake I made lies heavy in my heart, even more than one year later.
Thursday, June 27, 2013
Why I chose urology
A little background...
Its 7pm. I pick up the phone. I dial the number. The phone rings once, I panick and hang up.
I stare at my phone. Can I do this?
I'm lost in one of those infinite moments, where you think a lifetime of thoughts and scenarios in the span of seconds. What will I say? How will they react?
My phone rings, the harsh tones startling me out of my revelry. They are calling back...
I'm about to do the hardest thing I have every done.
I am about to tell my parents I want to be a urologist...
Ok sorry for the overdramatization, it really wasn't that suspenseful. But is sure as hell felt like it. My parents are traditional more blue collar people. We are first generation immigrants, no-one in my family is a doctor. So for my parents it was a big deal when I got into med school, and they were super excited to tell our family and friends that their son was a cardiologist, an emergency room doctor, etc.
So when I finally built up the nerve and told them, they weren't exactly thrilled. They didn't fully understand what it meant to be a urologist. Their impression was that urologists were essentially gynecologists for males.
But really, urology is an amazing field. First and foremost - urology is a surgical subspecialty. You have to love surgery. And I love being in the OR. As I detailed in a previous post, for me nothing beats being in the operating room. Urology affords me that opportunity.
But additionally, their are some specific things I love about urology.
Anatomy
I like the anatomy. I like the abdomen and pelvis, I like working the abdomen. I like being the master of all things urological (kidney/bladder/ureter/scrotum). We do our own ultrasounds, we read our own CT's, we do our own retrogrades in the OR. We are better at radiology in that sense.
Ownership
What do I mean by this? I think an example is best. A colorectal surgeon will get referred all his cases. GI treats the inflammatory bowel patients, when they fail medical management send them to the surgeon, he chops it out and sends them back to GI. Same thing with cancer.
But urology, we own our patients in a unique way. Sure we have the cancer referrals that we operate on and then lose. But we also have a huge population of patients that we manage. We are men's health doctors. We do annual exams, treat men for their ED, follow patients BPH (big prostate) voiding issues. Right now when I'm in clinic with my attendings, almost on a daily basis we take care of patients that he has been seeing for 10+ years. He's operated on them, managed them medically, and really know them. I like that about urology, we build very long relationships with our patients.
Master of our domain
We are masters of our domain (does anyone know that reference from Seinfeld??)
We medically AND surgically manage diseases of urological organs. We take care of BPH, recurrent UTI's, and stones, along with multiple others. I like being the guy that does that. I like to go to a patient and say well you have a stone, we can try medical or surgical management, but either way I'll be taking care of you. This ties in with anatomy and ownership, we really do take care of our patients from start to finish.
Hours:
I can honestly tell you that everyone for everyone who goes into urology, this is a factor. Urology is a surgical subspecialty, but we have far better hours than our general surgery brethren. Theirs are significantly fewer urological emergencies. Plus urology is alot less baby sitting, and we don't take care of the painful trauma bombs. Sure emergencies can be fun and exciting, but in thirty years will I still want to be doing that? Its kind of nice to have fewer emergencies, have a better schedule and more control over your life. Also our residency, while still grueling, is nowhere near as bad as our general surgery colleagues have it.
Diversity
I love this about urology. We do big open abdominal surgeries. We do a ton of laparoscopic surgery. We use the robot more than any other specialty, and have a good reason for using it. Our bread and butter is endoscopic surgery. Our pediatric surgeons are essentially plastic surgeons. The variety is huge.
People:
Urologists have a unique personality. First and foremost urology is a surgical subspecialty, so it attracts driven, intelligent, hard working type A personalities. At the same time though, almost paradoxically, we are some of the laid back, relaxed and funny people in the hospital. Jokes fly all the time in the OR, and in general we all have fun and don't take ourselves to seriously.
Theirs a reason that urology is so competitive these days, and I think the above outlines it. Its a fantastic field, full of people who love their job. When you love your job, you work harder to be better at it, and it just furthers the field.
AsConfucius said “Choose a job you love, and you will never have to work a day in your life.”
So when I finally built up the nerve and told them, they weren't exactly thrilled. They didn't fully understand what it meant to be a urologist. Their impression was that urologists were essentially gynecologists for males.
But really, urology is an amazing field. First and foremost - urology is a surgical subspecialty. You have to love surgery. And I love being in the OR. As I detailed in a previous post, for me nothing beats being in the operating room. Urology affords me that opportunity.
But additionally, their are some specific things I love about urology.
Anatomy
I like the anatomy. I like the abdomen and pelvis, I like working the abdomen. I like being the master of all things urological (kidney/bladder/ureter/scrotum). We do our own ultrasounds, we read our own CT's, we do our own retrogrades in the OR. We are better at radiology in that sense.
Ownership
What do I mean by this? I think an example is best. A colorectal surgeon will get referred all his cases. GI treats the inflammatory bowel patients, when they fail medical management send them to the surgeon, he chops it out and sends them back to GI. Same thing with cancer.
But urology, we own our patients in a unique way. Sure we have the cancer referrals that we operate on and then lose. But we also have a huge population of patients that we manage. We are men's health doctors. We do annual exams, treat men for their ED, follow patients BPH (big prostate) voiding issues. Right now when I'm in clinic with my attendings, almost on a daily basis we take care of patients that he has been seeing for 10+ years. He's operated on them, managed them medically, and really know them. I like that about urology, we build very long relationships with our patients.
Master of our domain
We are masters of our domain (does anyone know that reference from Seinfeld??)
We medically AND surgically manage diseases of urological organs. We take care of BPH, recurrent UTI's, and stones, along with multiple others. I like being the guy that does that. I like to go to a patient and say well you have a stone, we can try medical or surgical management, but either way I'll be taking care of you. This ties in with anatomy and ownership, we really do take care of our patients from start to finish.
Hours:
I can honestly tell you that everyone for everyone who goes into urology, this is a factor. Urology is a surgical subspecialty, but we have far better hours than our general surgery brethren. Theirs are significantly fewer urological emergencies. Plus urology is alot less baby sitting, and we don't take care of the painful trauma bombs. Sure emergencies can be fun and exciting, but in thirty years will I still want to be doing that? Its kind of nice to have fewer emergencies, have a better schedule and more control over your life. Also our residency, while still grueling, is nowhere near as bad as our general surgery colleagues have it.
Diversity
I love this about urology. We do big open abdominal surgeries. We do a ton of laparoscopic surgery. We use the robot more than any other specialty, and have a good reason for using it. Our bread and butter is endoscopic surgery. Our pediatric surgeons are essentially plastic surgeons. The variety is huge.
People:
Urologists have a unique personality. First and foremost urology is a surgical subspecialty, so it attracts driven, intelligent, hard working type A personalities. At the same time though, almost paradoxically, we are some of the laid back, relaxed and funny people in the hospital. Jokes fly all the time in the OR, and in general we all have fun and don't take ourselves to seriously.
Theirs a reason that urology is so competitive these days, and I think the above outlines it. Its a fantastic field, full of people who love their job. When you love your job, you work harder to be better at it, and it just furthers the field.
AsConfucius said “Choose a job you love, and you will never have to work a day in your life.”
Sunday, March 17, 2013
Trauma call
For the past month I've been on trauma nights. In our residency we do two months of nights, my first month was in the beginning of residency as I've talked about, and I'm doing my second month now. Before I was a med student, before I was a resident if someone told me "trauma nights" I would think it was the coolest thing in the world. In fact that happened recently, we had a bunch of friends over one Sunday, and as I got ready to go to work on Sunday evening everyone was saying how awesome it must be to be on trauma. I tried to explain how depressing it is, but stopped before I said anything stupid. Grey's anatomy, House, Scrubs - they've all made life as a doctor and surgeon out to be something it isn't. In those shows, the terrible traumas come in, but in the end everything works out. Shit isn't real. But it hits in you in trauma nights how real things are.
A little background on trauma. The ED handles the vast majority of simple trauma without activating the trauma pager. IE you have a car accident, you hurt your hand, no other injuries - that won't be a trauma. But, if its a bad accident, essentially any thought that surgery needs to be involved then the trauma pager is activated. You gotta remember, if someone unstable after a trauma, they are tanking in the field, an ED doctor can't do all that much other than acutely stabilize the patient. You need a surgeon, and its best to have the surgery team at the bedside waiting for you so as soon as you get in we're ready to roll. So when that trauma pager goes off, we haul ass down the trauma bay and get ready. We always expect the worst. We are notified whether its a level 1 or 2 trauma. Level 2 are generally stable, still a significant enough impact to activate a trauma but generally not someone who you expect to die any second (but you never know). A level 1 is serious, you have no idea what you're going to get but its generally bad. For level 1 traumas we expect to immediately intubate (breathing tube), line them up with central lines, chest tube/thoracotomy trays ready. You just never know. Its better to have a trauma surgeon and the team available then not. One of the memorable traumas: (identifying details obviously changed)
Its 7PM, Tuesday night. I'm running around the hospital, answering pages, doing post op checks. I was hoping for a quiet night, the thing with trauma nights is that if their are no traumas, by midnight you can be done with all your work and get some good rest as long as no floor patients are crapping out. So anyways I'm on the floor when the trauma pager goes off. The sound of that pager always gets my HR going, scares the hell out of me. Its a level 2, so me and my med student head down the trauma bay right away. All I'm thinking of is the work that I have to do, and hoping this trauma isn't too bad.
I get my lead on (we always take xrays in the trauma bay and as the intern, I stay with the patient during the xray), throw on some gloves and wait to hear whats coming in. The ED nurse tells us its a pedestrian hit by car. This is one of the most common traumas we get. Me, my chief resident and the ED attending are just hanging out in the trauma bay waiting, joking around. Finally about 10 minutes later the ED doors bang open and paramedics are rolling the trauma in. They yell "22 year old female, jogging, struck by car ~20 mph". We transfer her to the trauma bed and get to work. We are a well oiled machine, consisting of the chief resident, junior resident, and myself (the intern). The junior resident starts with the ABC (if you remember from CPR, just make sure their breathing and airway is intact), while I help the nurses get the BP cuff/EKG leads on for our first set of vitals. While the junior completes the head to toe assessment I start cutting off all the patients clothes. Trust me - you never want to be a trauma, no privacy, no dignity. We cut everything off.
Her vitals were stable, she was alert and oriented with no obvious life threatening injury so we all slow down a bit. We do a FAST abdominal ultrasound exam, which tells us if their is a large amount of free fluid in the abdomen which would imply an urgent trip to the operating room. Its negative. Because she lost consciousness in the field, we decide to get a CT of the head and cspine just to be safe. We roll her over to CT, grab a seat and wait for the scans. This is what we see:
She had a huge epidural hematoma (brain bleed). As med students we see these pictures a hundred times, and I had seen a couple of subtle ones on traumas before. This one wasn't subtle (Obviously that picture is not her, its from google, but it was that big). She had midline shift and everything, yet her neuro exam was perfect. We call neurosurg right away, they come down, evaluate her, and recommend sending her to the neurosurgery ICU and watch her closely.
Why did this trauma stick out in my head? Well after the CT, but before she went to the neurosurg ICU she had a bunch of lacerations that needs to be sutured in the trauma bay, nothing unusual and the task usually falls to the intern. We also had some time where I had to stay with her while the transfer to the ICU was being sorted out; the team didn't want to leave her alone unmonitored. So we start talking, and it kinda hit me how completely normal she was. Its this 22 year old girl from Europe who came to LA to work in fashion. She was just out for a jog and thinking about her weekend plans.
Working in this field, seeing all the trauma's roll in one after another you lose a sense of the human connection. The traumas, the patients are just work. We don't even assign them real names, they have trauma code words (oftentimes traumas who come in don't have ID and we can't ask them their name, so by default all traumas get assigned a code word). You lose empathy, start to identify the patients by their disease process. We don't say "how is mr jones doing", we say "how's the old guy who had the splenectomy doing".
But talking to that girl I saw how scared she was, she kept on thanking us but she as clearly in shock at what was happening. We never stay with out patients long enough to talk to them about anything but the acute medical/surgical problems; the social workers/nurses/therapists/case managers are the ones who figure the "other stuff" out. She had emergent surgery that night to evacuate the hematoma, she was going to have a serious scar and probably a long recovery.
But the main point here I think is that I understand why we don't try and connect with our patients. It would destroy you. We get so many drunk people who come in after doing something stupid - hell not too many years ago that could have easily been me or my friends. We never empathize with them, we call em drunken idiots and try to get em out of the ED as soon as possible. For all the terrible motor vehicle traumas we see and don't think about, man we all drive to work. That could be our family, our friends, us. We never think like that; its just a job. And it has to be like that because like any other thing in life sometimes things don't go well, bad things happen that are out of your control. And sometimes bad things happen because you or someone on your team screwed up. And if you treat this like more than a job, if you stop and actually put yourself in the patients shoes or if you try to treat everyone like you would treat your mom or dad I really think you will lose your mind. If you thought about the consequences your actions had on peoples lives, I don't think I could bear it.
And that sobering thought, the idea that I treat work like work I think has really defined my intern year. I know lots of people think that we become doctors for women, power, and money - but really thats not what drove me and most people I know to do medicine. I worked in tons of menial jobs in high school and college, and what made me want to do medicine was the idea that I could get paid, my career would be doing something intellectually stimulating, interesting, and I'd be helping people. I like to think I'm a genuinely nice guy who cares about others. I've always been that way. I remember as a medical student spending hours with patients, talking to them. I really empathized, and I couldn't understand why residents and attendings were so callous, so rushed (their will actually be another post about a patient from my third year of medical student that really changed me). I remember thinking I'd never be like that...
And then I think of how am I know. I'm just 8 months into my residency, and already I'm losing that emotional touch. I just want to get through the day. When the trauma pager goes off, my mindset isn't f**k someone may be badly injured, its f**k I hope its not too bad so MY day isn't ruined by this. It sucks, and its just not surgery its all specialties. We all try and dump patients on other services. No-one wants to sit down and figure out the social situation, the background, we want to just get on with our day. We have the same mentality with the hospital that virtually everyone has with their daily job. The only difference is instead of have that attitude towards meetings, the bottom line, clients, customers etc that is completely acceptable in any other profession we have that attitude towards sick human beings who are coming to us for help.
Every once in a while something reminds me of how I used to be, how much I used to empathize. And please don't get me wrong, myself and most people in our field are genuinely good people. We do want whats best for our patient. Thats the underlying sentiment, thats what drives us. But this damn system, you are so overworked, so tired, so stressed that sometimes you lose sight of the big picture. I work in an era where work hours are significantly improved from where they used to be, but its still nothing like 99% of the population will ever experience. I easily hit 40 hours by Wed afternoon. I go the entire year averaging about 80 hours a week of work. I get one day off a week, and its sometimes in the middle of the week. We don't get many holidays, and tend to be on call for most of them anyways. But the point of this post isn't to complain, because honestly I still think I'm blessed to be in the position I'm in and wouldn't trade it for anything. But this system changes you, and not for the better. I know I'm still that person that cares, that I would do anything for my patient. I just need to remind myself of that sometimes...
A little background on trauma. The ED handles the vast majority of simple trauma without activating the trauma pager. IE you have a car accident, you hurt your hand, no other injuries - that won't be a trauma. But, if its a bad accident, essentially any thought that surgery needs to be involved then the trauma pager is activated. You gotta remember, if someone unstable after a trauma, they are tanking in the field, an ED doctor can't do all that much other than acutely stabilize the patient. You need a surgeon, and its best to have the surgery team at the bedside waiting for you so as soon as you get in we're ready to roll. So when that trauma pager goes off, we haul ass down the trauma bay and get ready. We always expect the worst. We are notified whether its a level 1 or 2 trauma. Level 2 are generally stable, still a significant enough impact to activate a trauma but generally not someone who you expect to die any second (but you never know). A level 1 is serious, you have no idea what you're going to get but its generally bad. For level 1 traumas we expect to immediately intubate (breathing tube), line them up with central lines, chest tube/thoracotomy trays ready. You just never know. Its better to have a trauma surgeon and the team available then not. One of the memorable traumas: (identifying details obviously changed)
Its 7PM, Tuesday night. I'm running around the hospital, answering pages, doing post op checks. I was hoping for a quiet night, the thing with trauma nights is that if their are no traumas, by midnight you can be done with all your work and get some good rest as long as no floor patients are crapping out. So anyways I'm on the floor when the trauma pager goes off. The sound of that pager always gets my HR going, scares the hell out of me. Its a level 2, so me and my med student head down the trauma bay right away. All I'm thinking of is the work that I have to do, and hoping this trauma isn't too bad.
I get my lead on (we always take xrays in the trauma bay and as the intern, I stay with the patient during the xray), throw on some gloves and wait to hear whats coming in. The ED nurse tells us its a pedestrian hit by car. This is one of the most common traumas we get. Me, my chief resident and the ED attending are just hanging out in the trauma bay waiting, joking around. Finally about 10 minutes later the ED doors bang open and paramedics are rolling the trauma in. They yell "22 year old female, jogging, struck by car ~20 mph". We transfer her to the trauma bed and get to work. We are a well oiled machine, consisting of the chief resident, junior resident, and myself (the intern). The junior resident starts with the ABC (if you remember from CPR, just make sure their breathing and airway is intact), while I help the nurses get the BP cuff/EKG leads on for our first set of vitals. While the junior completes the head to toe assessment I start cutting off all the patients clothes. Trust me - you never want to be a trauma, no privacy, no dignity. We cut everything off.
Her vitals were stable, she was alert and oriented with no obvious life threatening injury so we all slow down a bit. We do a FAST abdominal ultrasound exam, which tells us if their is a large amount of free fluid in the abdomen which would imply an urgent trip to the operating room. Its negative. Because she lost consciousness in the field, we decide to get a CT of the head and cspine just to be safe. We roll her over to CT, grab a seat and wait for the scans. This is what we see:
She had a huge epidural hematoma (brain bleed). As med students we see these pictures a hundred times, and I had seen a couple of subtle ones on traumas before. This one wasn't subtle (Obviously that picture is not her, its from google, but it was that big). She had midline shift and everything, yet her neuro exam was perfect. We call neurosurg right away, they come down, evaluate her, and recommend sending her to the neurosurgery ICU and watch her closely.
Why did this trauma stick out in my head? Well after the CT, but before she went to the neurosurg ICU she had a bunch of lacerations that needs to be sutured in the trauma bay, nothing unusual and the task usually falls to the intern. We also had some time where I had to stay with her while the transfer to the ICU was being sorted out; the team didn't want to leave her alone unmonitored. So we start talking, and it kinda hit me how completely normal she was. Its this 22 year old girl from Europe who came to LA to work in fashion. She was just out for a jog and thinking about her weekend plans.
Working in this field, seeing all the trauma's roll in one after another you lose a sense of the human connection. The traumas, the patients are just work. We don't even assign them real names, they have trauma code words (oftentimes traumas who come in don't have ID and we can't ask them their name, so by default all traumas get assigned a code word). You lose empathy, start to identify the patients by their disease process. We don't say "how is mr jones doing", we say "how's the old guy who had the splenectomy doing".
But talking to that girl I saw how scared she was, she kept on thanking us but she as clearly in shock at what was happening. We never stay with out patients long enough to talk to them about anything but the acute medical/surgical problems; the social workers/nurses/therapists/case managers are the ones who figure the "other stuff" out. She had emergent surgery that night to evacuate the hematoma, she was going to have a serious scar and probably a long recovery.
But the main point here I think is that I understand why we don't try and connect with our patients. It would destroy you. We get so many drunk people who come in after doing something stupid - hell not too many years ago that could have easily been me or my friends. We never empathize with them, we call em drunken idiots and try to get em out of the ED as soon as possible. For all the terrible motor vehicle traumas we see and don't think about, man we all drive to work. That could be our family, our friends, us. We never think like that; its just a job. And it has to be like that because like any other thing in life sometimes things don't go well, bad things happen that are out of your control. And sometimes bad things happen because you or someone on your team screwed up. And if you treat this like more than a job, if you stop and actually put yourself in the patients shoes or if you try to treat everyone like you would treat your mom or dad I really think you will lose your mind. If you thought about the consequences your actions had on peoples lives, I don't think I could bear it.
And that sobering thought, the idea that I treat work like work I think has really defined my intern year. I know lots of people think that we become doctors for women, power, and money - but really thats not what drove me and most people I know to do medicine. I worked in tons of menial jobs in high school and college, and what made me want to do medicine was the idea that I could get paid, my career would be doing something intellectually stimulating, interesting, and I'd be helping people. I like to think I'm a genuinely nice guy who cares about others. I've always been that way. I remember as a medical student spending hours with patients, talking to them. I really empathized, and I couldn't understand why residents and attendings were so callous, so rushed (their will actually be another post about a patient from my third year of medical student that really changed me). I remember thinking I'd never be like that...
And then I think of how am I know. I'm just 8 months into my residency, and already I'm losing that emotional touch. I just want to get through the day. When the trauma pager goes off, my mindset isn't f**k someone may be badly injured, its f**k I hope its not too bad so MY day isn't ruined by this. It sucks, and its just not surgery its all specialties. We all try and dump patients on other services. No-one wants to sit down and figure out the social situation, the background, we want to just get on with our day. We have the same mentality with the hospital that virtually everyone has with their daily job. The only difference is instead of have that attitude towards meetings, the bottom line, clients, customers etc that is completely acceptable in any other profession we have that attitude towards sick human beings who are coming to us for help.
Every once in a while something reminds me of how I used to be, how much I used to empathize. And please don't get me wrong, myself and most people in our field are genuinely good people. We do want whats best for our patient. Thats the underlying sentiment, thats what drives us. But this damn system, you are so overworked, so tired, so stressed that sometimes you lose sight of the big picture. I work in an era where work hours are significantly improved from where they used to be, but its still nothing like 99% of the population will ever experience. I easily hit 40 hours by Wed afternoon. I go the entire year averaging about 80 hours a week of work. I get one day off a week, and its sometimes in the middle of the week. We don't get many holidays, and tend to be on call for most of them anyways. But the point of this post isn't to complain, because honestly I still think I'm blessed to be in the position I'm in and wouldn't trade it for anything. But this system changes you, and not for the better. I know I'm still that person that cares, that I would do anything for my patient. I just need to remind myself of that sometimes...
Subscribe to:
Posts (Atom)